A first-of-its-kind evaluation, led by researchers at UNSW’s Kirby Institute, demonstrates the real-world benefits of community-led molecular point-of-care (POC) testing for sexually transmissible infections (STIs) in remote Australia.
The results have been published in The Lancet Regional Health – Western Pacific.
Research on the national STI point-of-care testing program (previously known as TTANGO, or Test, Treat and Go) demonstrated more timely treatment of STIs was achieved following a positive point-of-care test compared with traditional laboratory testing – an outcome particularly significant for women. In addition, the research highlighted that the testing led to reductions in infectious days and fewer onward community transmissions, both substantial public health benefits.
It also showed that the high accuracy of point-of-care testing in remote primary care settings was maintained during the evaluation period and was similar to lab-based testing. Furthermore, the evaluation highlights that, when implemented in real-world settings, point-of-care testing sees similar results as in a controlled trial.
What are the benefits of more timely treatment of STIs?
For women, some “silent STIs” such as chlamydia and gonorrhoea mean that, often, the infections can go unnoticed and untreated, which can lead to other serious health concerns. Being diagnosed quickly and receiving faster treatment means women are less likely to develop reproductive, maternal and neonatal complications of infection, including pelvic inflammatory disease (PID), ectopic pregnancy, infertility and poor pregnancy outcomes.
“The quicker you treat STIs, the less likely other concerns will develop,” says Dr Louise Causer, Senior Lecturer at the Kirby Institute and first author on the paper. “To put that in perspective, figures show that in remote regions of Australia, more than 40 percent of hospital admissions and emergency department presentations for pelvic inflammatory disease among young Aboriginal women are due to chlamydia or gonorrhoea infections.”
So, what exactly is TTANGO?
The TTANGO program was implemented by the Kirby Institute and the Flinders University International Centre for Point-of Care Testing, in partnership with Aboriginal community-controlled health organisations (ACCHOs) and their member health services, government, and pathology providers.
The TTANGO trial launched in 2013, introducing molecular point-of-care testing for STIs in remote primary care settings and supporting clinicians to use the latest technology in STI testing. It aimed to improve the diagnosis and treatment of chlamydia and gonorrhoea in remote Aboriginal and Torres Strait Islander communities across Australia by testing and diagnosing STIs within one visit.
Following the successful trial, the TTANGO2/3 program has seen the scale-up of testing from 2016 onwards, with the introduction of a test for trichomoniasis in 2018.
Currently, more than 75 rural and remote clinics in six states and territories nationally take part in the program and lead the implementation of the new model.
The STI program continues now as the First Nations Molecular POC Testing Program.
Why is it so important?
Nationwide, young First Nations peoples – particularly those living in regional and remote communities – experience some of the highest rates of STIs worldwide. In fact, other studies have shown that just under half of all people living in remote communities aged 16-19 have an STI at any given time.
“There are a range of complex factors that impact sexual health in remote communities, including health service capacity, population mobility, and social and cultural factors around shame and stigma,” explains Robert Monaghan, Manager Aboriginal and Torres Strait Islander Health Research program. “A big contributing factor is the often-huge geographical distances between health services and laboratories, which can mean that when someone does attend a clinic for a test, it can take days or weeks for a result to be returned to the patient and if needed, treatment provided.”
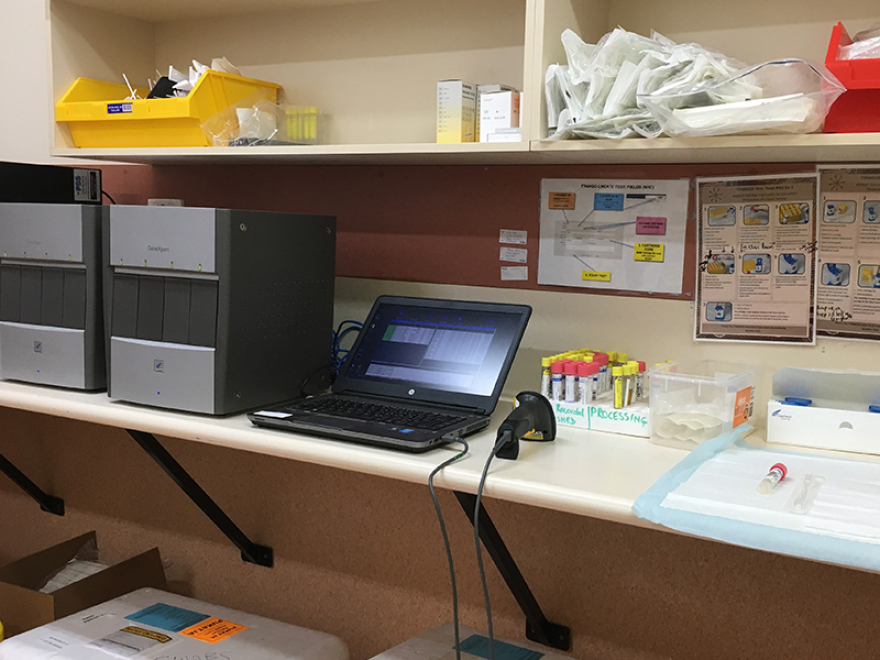
That’s where point-of-care testing comes in. It allows a health worker, nurse or doctor to perform a molecular test on a patient sample on-site at a health centre using a compact testing device, with results available in less than two hours. Treatment can then commence immediately in line with test results.
“Such a reduction in the time between testing and treatment of STIs has multiple benefits,” adds Dr Causer. “As well as obviously benefitting the health of individuals, timely treatment also positively impacts public health due to reduced onward transmission and a reduction in health complications caused by certain STIs.”
Expansion is on the horizon
The evaluation demonstrates that supported by strong community leadership, operator training, competency assessment, quality management, and connectivity and technical support, STI point-of-care testing can be successfully scaled up and sustained.
The next steps? Further expand the number of clinics participating in the program and increase the number of tests performed to make sure all young people in regional and remote communities have access to this technology.
“The new Medicare rebate will help but more needs to be done to overcome other challenges including limited workforce capacity and encouraging young people to be tested,” says Dr Causer. “In addition, in partnership with the National Aboriginal community-controlled health organisation (NACCHOs), ACCHOs and other stakeholders, we are exploring the value of point-of-care testing for other important conditions in remote communities including respiratory infections, human papillomavirus (HPV) and Group A streptococcal infection.
“The benefits of point-of-care testing for STIs will make a big difference to the health and wellbeing of young people in regional and remote communities, but without the strong relationships that have been built over the last decade, none of this would have been possible. Community-led health services on the frontline, together with our partners and other providers who really believe in the program, are what make it all happen.”