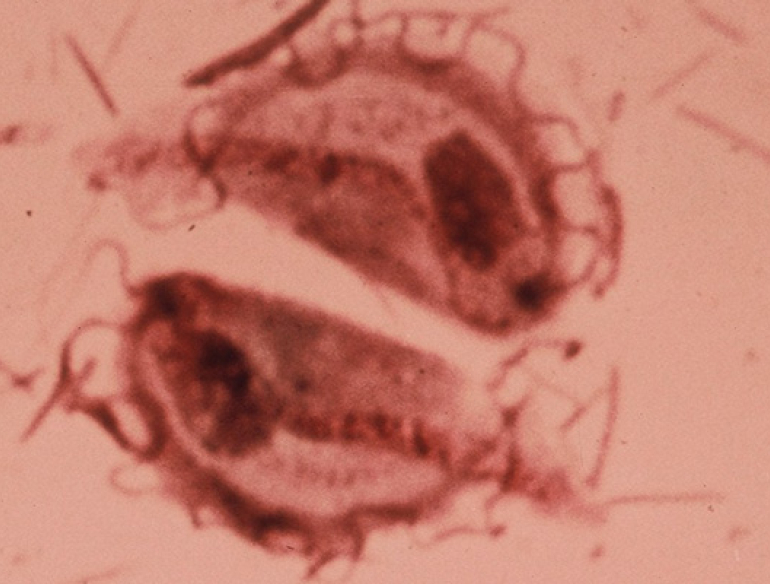
(SYDNEY, Wednesday 17 April 2019) A new study from the Kirby Institute at UNSW Sydney has found that with the move from pap smear to DNA testing for human papillomavirus (HPV) to prevent cervical cancer, there is risk that a now rare sexually transmissible infection (STI), Trichomonas vaginalis (TV), could increase among Australian women.
The Kirby Institute’s Professor Basil Donovan is a big a supporter of the transition to an HPV-DNA test. “This is a far better test than the pap smear. It is an important innovation in our strategy to achieve cervical cancer elimination in Australia.
“However, the change from a pap smear to a DNA test means technicians no longer examine specimens under the microscope. It was during this examination that we were able to opportunistically identify rare cases of TV and treat it,” said Professor Donovan, who is head of the Kirby Institute’s Sexual Health Program.
The results of the mathematical modelling study were published in the journal Sexually Transmitted Infections today and suggest that the risk of a return of TV could be avoided with routine screening alongside a chlamydia test.
In 2017, Australia transitioned from a two-yearly pap smear screening program to a five-yearly HPV DNA test-based cervical screening program, commencing for women aged 25 years old. While both tests take a sample of cells from the cervix, the new tests looks for HPV (the cause of the overwhelming majority of cervical cancers), rather than cell abnormality.
TV is an STI that causes a range of morbidities, including pre-term labour and pelvic inflammatory disease. TV rates are very low in Australian cities, partly due to opportunistic detection during pap smears. Previous research by the Kirby Institute predicts that TV prevalence could increase sixfold over 20 years under the new cervical screening program, if not supplemented by additional strategies to detect asymptomatic TV infection.
“STI screening guidelines in Australia recommend annual chlamydia tests for sexually active people aged 16-30, and this is a very good opportunity to include a TV test.” said Associate Professor David Regan from the Biostatistics and Databases Program at the Kirby Institute. He is the lead-author on the paper.
“Our modelling showed that routine testing for TV with a chlamydia test would substantially reduce the rate of increase in TV compared with no supplemental testing,” said Associate Professor Regan. “However unfortunately, because chlamydia testing rates in Australia are below optimal levels, we would still see a gradual increase in TV. This means that TV screening needs to be considered alongside strategies to enhance STI testing overall, as well as enhanced national surveillance systems.”
Professor Jane Hocking, Head of the Sexual Health Unit in the School of Population and Global Health at the University of Melbourne says it is essential that any strategy to enhance TV testing works to reassure women of the necessity and safety of the current HPV-DNA screening program, and supports the important strides we’ve made in cervical cancer prevention in Australia.
“Cervical cancer is a much more dangerous, life threatening disease than TV. The screening program we have in Australia is world-class, and together with HPV vaccination, it means Australia is realistically looking to eventually eliminate cervical cancer,” said Professor Hocking.
“We’re lucky in Australia to have extensive STI testing and surveillance systems in place. This study shows us that with routine screening, increased health promotion activities and enhanced surveillance systems, TV will continue to be an uncommon STI in urban Australia.”
Contact
Luci Bamford
Phone
0432 894 029